Welcome to BAZAAR.com's first ever Period Month, where for an entire four weeks we'll be publishing stories devoted to your period. Our aim is to delve into what really happens during a woman's cycle—and with the help of Flo Living founder Alisa Vitti, we'll teach you how you can harness your hormones as a path to success, power and global change.
My phone finally rang. It was the call I had been anxiously waiting for: the results of the transvaginal ultrasound I had undergone a few days earlier. “So, hmph, how can I say this?” My primary care doctor sighed and took a pregnant pause. My stomach dropped. This is it, I thought. I am dying. I have cancer.
Initially, I went to see my doctor a few weeks after first experiencing a sharp but fleeting pain in my lower abdomen that later turned into a dull and persistent ache. I ignored it at first—it was probably nothing. Maybe it’s gas or stress. Maybe it’s my birth control being weird. But as the days went on, I started to worry that maybe there was something seriously wrong.
My doctor suggested a transvaginal ultrasound out of an abundance of caution. And even though I played out the worst-case scenario in my head over and over, I never imagined the test results would actually be abnormal. “So everything is fine, it looks good, um, but they did see something on the ultrasound results called adenomyosis,” my doctor explained. She was clearly still reading and processing the results in real time, hence the overly dramatic delivery. Is that bad? I asked, while simultaneously trying to figure out how to spell adenomyosis so I could Google it. I had never heard of adenomyosis. But it didn’t sound like a good thing.
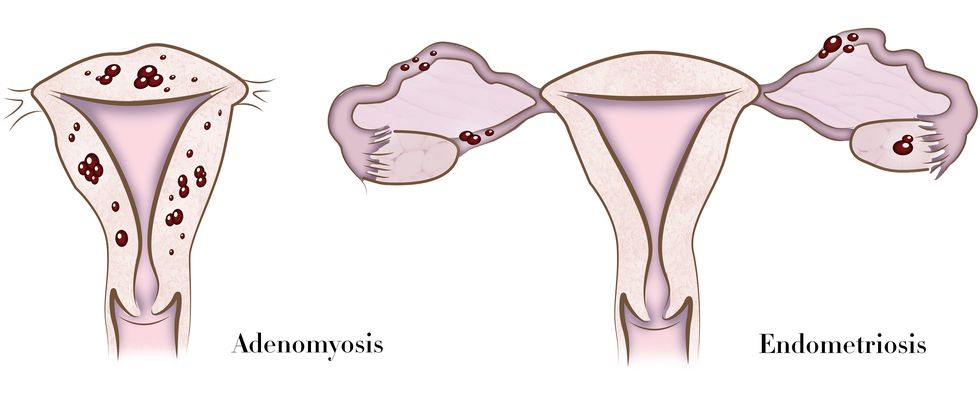
My doctor tried to quell my fears by explaining it’s merely an unusual thickening or hardening of the uterine wall caused by the glandular tissue being pushed into the muscle. It’s not cancer, it’s not going to turn into cancer, and we probably would have never known about it had I opted out of the ultrasound. The only known cure? A hysterectomy. She assured me not to worry about it yet—but it wouldn’t hurt to have a conversation with my gynecologist. So I called up my OBGYN’s office, and she was just as confused as I was to hear about the diagnosis. “You’re much too young for that,” she told me. She also advised to put any concerns about it aside. Pregnancy and fertility could be an issue, she said, since a hard uterus can’t grow a baby to term, and miscarriages would likely be in my future, but I could worry about that later—when I was actually ready to start a family, she added. (Though other doctors I spoke with later stressed that this is a hypothesis and not a proven theory.) “Just stay on birth control for now, and we’ll discuss that in a few years,” she said matter of factly. Her calm demeanor didn’t really mirror the gravity of the news she had just dropped on me.
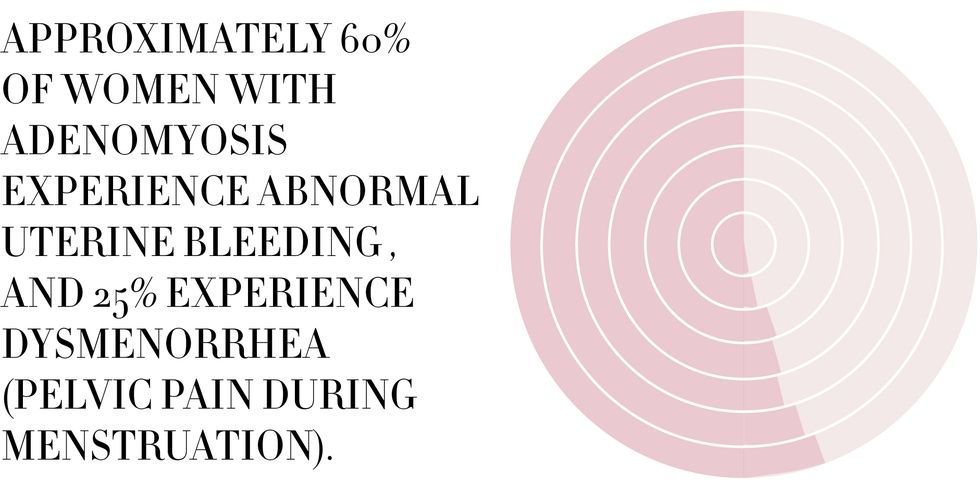
The more I read about adenomyosis, the more apparent it became that it wasn’t just the cause of that one persistent, dull pain—but also of my years of menstrual suffering (heavy periods, clotting, painful cramping). And after scouring every corner of the internet looking for answers and speaking with several experts, something even more concerning became clear: I’m not sure the medical community even knows the extent to which the condition affects women of all ages. Like many women’s health issues, not only is adenomyosis understudied, it’s also misunderstood. “We’re in a period of time where we’re recognizing that maybe it’s more common than we thought,” says Dr. Cynthia Austin, an obstetrician-gynecologist at Cleveland Clinic in Ohio. “We’re still in the area where things are evolving in regards to diagnosis, what it causes, and what you should do to treat it.”
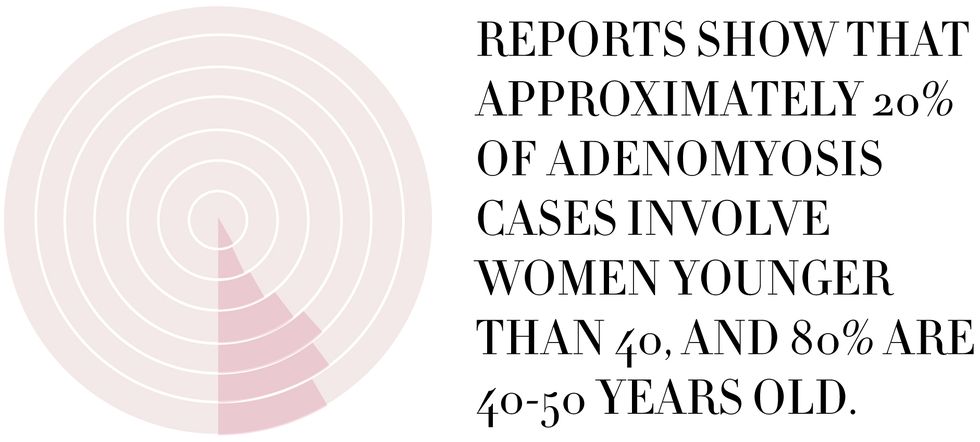
Imaging devices like MRIs and ultrasounds can suggest the presence of it, but the only true route to a diagnosis is with a total removal of the uterus, which is why it might be wildly underreported in women under the age of 40 (studies have found 80 percent of cases are diagnosed in women between the ages of 40 and 50 years-old). “Adenomyosis is kind of similar to endometriosis: a lot of women have it, but a lot of them don’t have symptoms,” says Dr. Lisa Dabney, Assistant Professor of Obstetrics, Gynecology and Reproductive Science, at Mount Sinai in New York. The difference between the oft-mentioned endometriosis and adenomyosis is that the latter occurs within the uterine muscle itself, making it impossible to treat with surgery. “The hard part is that you can’t really do anything—you can’t fix it,” said Dr. Dabney. “You can treat heavy periods but you can’t get rid of adenomyosis without a hysterectomy. That’s why we don’t look for it [as doctors] because we can’t do anything about it.”
Talk about a bleak outlook. Sometimes doctors don’t even tell the patient about it because it’s deemed clinically insignificant. “People often think that with modern medicine, everything can be fixed. No, actually, a lot of things can’t be fixed but we can do a lot to minimize people's symptoms,” explained Dr. Dabney. “I really would stress that even though it’s not treatable [with Western medicine], in most women it’s not going to impact them. Most people don’t need to freak out about it.” I wasn’t freaked out—but the one thing I couldn’t understand was why I had never even heard of the condition. Nobody around me knew what it was, and they all had uteruses! I spent my teenage years suffering through excruciating periods thinking it was normal—par for the course of being a woman. But periods aren’t supposed to bring along crippling pain?
"You’re walking around thinking this is what it’s like to have a period, when really, it’s not. We need a perspective shift,” explained Alisa Vitti, a functional nutritionist, women’s hormone expert, author of WomanCode, and creator of the Flo Living Hormone Center. “As women we’re taught that there’s nothing to be done. It’s supposed to suck, periods are terrible—but that’s not accurate or biologically sound at all.” Vitti, who says a bad period is a sign that our own hormones are totally out of whack, strongly believes that doctors need to stop doling out birth control as the magical cure to everything menstrual and uterine-related—especially in women as young as 13 and 14. By masking the symptoms with artificial hormones, we’re never actually getting to the root of the problem.
Almost proving Vitti’s point, my doctor almost immediately insisted that I continue popping my levonorgestrel-based birth control pills (I take Quasense, a generic form of Seasonale) for as long as I didn’t want children. “Birth control is a good way to control endometriosis, and in theory, control adenomyosis,” said Austin, explaining that pills suppress the natural hormone levels in your body by pumping it with a measured dose of synthetic hormones instead, meaning the conditions theoretically won’t grow or flare—the cover-up of symptoms Vitti mentioned. Both Austin and Dabney also recommend the Mirena IUD as another option to keep the symptoms in check. The hormones in birth control pills have to travel through your stomach and liver before they reach your uterus; IUDs deliver high doses right to the source of the growth, so they might be more effective at halting abnormal growth while simultaneously minimizing your symptoms. Again, though, no one knows for sure, because there simply isn’t enough research to back these theories up.
Another fertility-sparing treatment option for adenomyosis is something called Lysteda. It’s a form of tranexamic acid that was first used years ago as a blood-clotting agent for soldiers on the battlefield. The drug is now prescribed in the U.S. to women with heavy periods, but it can’t be taken with hormone-releasing birth control since it compounds the risk for blood clots. “It’s non-hormonal, it only affects your blood’s clotting abilities, and you only take it when you’re bleeding. Which is kind of a nice feature—you don’t have to take something every day,” noted Dabney.
It’s been almost three years since my unexpected diagnosis, and I continue to numb my symptoms with birth control, just like my doctor ordered, and just like I have for the last nine years. Birth control has rendered me period-less for all intents and purposes: I bleed for about a day once every three months, with no PMS-induced emotional breakdowns. I was once the girl you could always count-on to pass you a tampon; now I rarely need more than a lightweight liner on my worst day. Yet it’s worth noting that my flare-up of adenomyosis occurred while I was on the pill, albeit under a time of unusually intense stress. I’ve never seen birth control as a long-term solution. I’ll have to go off of it eventually, and then what? Will the painful, frustrating periods rear their bloody head the second I do? It’s likely. The medical community told me that adenomyosis is something I will likely live with, symptomatic or not, forever—or, until I opt for a hysterectomy. Surely there is a better way.
According to Vitti, the immune system—as well as the nutrients in food women consume—plays a big part in reproductive issues, and the fact a hysterectomy is the only option presented to women with endo, ando and PCOS by doctors completely dumbfounds her. Vitti prescribes a specific diet to her patients, which in turn supports the functioning of the endocrine system (the collection of glands that regulate your hormones) in the order and sequence it needs to be. “By addressing the immune system and the hormone system [through diet] you can really be symptom-free,” she explains. The nutrients we ingest affect each of us through complex processes that can be difficult to understand (did you know certain vegetables like kale and brussels sprouts can aid our bodies in breaking-down estrogen?). Once you dig deeper into female biology, a “roadmap” for for how we should be eating becomes clear, says Vitti, and it’s all based on where we stand in our 28-day cycle. The first thing she told me on the phone? Drop the coffee—right now. “Any women with a menstrual disorder should not be touching caffeine. It’s so disruptive. The science is overwhelming—caffeine increases the formation of cysts and inflammation that we see on the ovaries, uterus, and breast tissue. Especially if you have a diagnosis of something with cysts or tumors, it’s 100% not a negotiable. You’ve got to get rid of it,” she says.
Vitti believes that endometriosis, adenomyosis, PCOS, and a host of other conditions can be dieted into remission by eating specific healthful foods—while also cutting out foods that create a hormone imbalance. That means no gluten, dairy, coffee, or pizza—and you can all but forget about alcohol. Any substance that triggers an inflammatory response, screws with your cortisol production, throws off your blood sugar levels, or pumps your body full of faux estrogen (i.e. birth control) should be forbidden. Hormone-related conditions feed off a body imbalanced, she says, and only then will you finally feel what it’s like to be a woman in complete control of her own body and cycle.
I’ve made baby steps toward adopting Vitti’s female-focused diet, but my biggest hurdle remains to be The Pill. Vitti’s plan can’t do much for me while I’m still on it, since it’s synthetically regulating my hormones. I’m eating more plant-based foods than ever before, and I’m weaning myself off off meat and dairy to try and cut-back on the amount of additional hormones I’m ingesting (unless they are hormone-free organic and grass-fed options). But I can’t bring myself to quit birth control just yet, partially out of fear of pregnancy. Though Vitti does note that a balanced hormonal body should mean my period would come so regularly that I’d be able to expect it within an hour—and contraception and ovulation, when your body operates with Swiss precision, thus becomes much easier to navigate.
I also can’t quit the pill partially out of my blind faith for Western medicine. Going off it would mean breaking the advice of several doctors, who swear it’s the best thing out there for keeping adenomyosis in-check. This is something Vitti hopes to see change in her lifetime: doctors actually discussing how effective diet can be at fixing hormonal imbalances—rather than doling out the pill as a blanket quick-fix prescription for women. Recently, Vitti even wrote an open letter to Lena Dunham, who suffers from endometriosis and believes the pill is her only answer to a life without pain. “It’s particularly distressing to me, because I know that you can do something about endometriosis, the pain and everything that comes along with this health issue,” Vitti wrote to Dunham last year.
As I head into my childbearing years, I can’t help but worry about my reduced chances of fertility. Who do I put my faith into? My team of doctors or the likes of Vitti? Even though I’m left with more questions about adenomyosis than answers, I’m grateful the condition was brought to my attention and not brushed aside as a blip on the ultrasound. It vindicates all those days, weeks and years when I was suffering in pain and thought it was just part of the deal of being born a woman. If this diagnosis has taught me anything, it’s that arming yourself with a deeper understanding of your own biology is the very first step in helping yourself.